Listening to Parkinson's Patients: Nonmotor Symptoms Take Center Stage as Researchers Gather Intel on Patients’ Unmet Needs
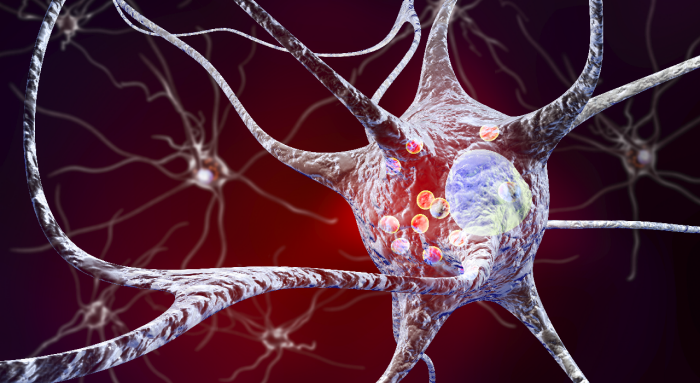
Parkinson's disease is a complex and multifaceted disorder.1 While the motor symptoms – tremors, slowness in movements and rigidity – tend to be the most recognizable, almost all people with Parkinson's also experience a plethora of nonmotor symptoms, and these symptoms often have a substantial and negative impact on quality of life.2,3
There is growing awareness within the medical community of the significance of nonmotor symptoms, and there is a movement within the Parkinson’s research community to better understand how nonmotor symptoms impact patients’ daily living. Researchers now are exploring how to gather information on patient needs and design clinical trials that focus on achieving improvement in daily activities and quality of life – a measure that may ultimately be more meaningful than improvement in a particular symptom.
“We need a deeper understanding of what patients think and what their needs are – what are the most bothersome symptoms and how do those symptoms impact their activities of daily living?” says Didier Meulien, MD, lead medical specialist in neurology clinical development at Lundbeck, the only global biopharmaceutical company focused solely on the brain. “Understanding what matters most to patients is a hallmark of Lundbeck’s research programs, and we are committed to advancing new Parkinson’s treatment options that will have meaningful impact on people’s lives.”
A range of symptoms
Because Parkinson's is widely perceived to be a motor disorder, the first step to understanding the impact of Parkinson’s nonmotor symptoms is simply recognizing them. Neither people with Parkinson’s nor their healthcare providers may fully appreciate the range of nonmotor symptoms attributable to the disease or how they exhibit at various stages of the patient journey.
We need a deeper understanding of what patients think and what their needs are – what are the most bothersome symptoms and how do those symptoms impact their activities of daily living?
— Didier Meulien, MD, Lundbeck
Some nonmotor symptoms appear well before a Parkinson’s diagnosis – as many as 10 years prior, in some cases.4 However, nonmotor symptoms are often overlooked in this early stage and may not be connected to Parkinson’s.2 Early nonmotor symptoms include1,4:
- REM sleep disorder
- Constipation
- Depression
- Anxiety
- Reduced ability to smell (hyposmia)
- Taste loss
- Excessive sweating
- Excessive daytime sleepiness
As the patient journey progresses, additional nonmotor symptoms often appear along with the occurrence of motor symptoms. These include3,4, 5:
- Fatigue
- Cognitive impairment
- Pain
- Apathy
- Urinary dysfunction
- Sudden drops in blood pressure upon standing (neurogenic orthostatic hypotension)
- Hallucinations
- Dementia
Wide prevalence, significant unmet need
Research shows that virtually all Parkinson’s patients experience some or most of these nonmotor symptoms along their disease journey. According to one study, the mean number of nonmotor symptoms experienced by each patient was 10.5.6 Another patient survey revealed that nearly two thirds were plagued by fatigue, and more than half reported forgetfulness.7
To best meet the needs of people living with Parkinson’s, both researchers and healthcare providers must learn to focus on the full experience of patients with Parkinson's disease.
— Simona Sgarbi, PhD, Lundbeck
And these symptoms have significant impact on the quality of life of both patients and care partners. An internet survey on the impact of neurogenic orthostatic hypotension (nOH) found that most of the patients (87 percent) and care partners (95 percent) surveyed said that nOH symptoms had a negative impact on patients’ ability to perform certain daily activities.8 Additionally, more than half of the patients and 73 percent of the care partners reported that some daily activities were reduced or stopped because of symptoms of nOH.8
Another large study found that nonmotor symptoms actually have a greater impact on health-related quality of life than motor symptoms, and progression of these nonmotor symptoms contributes to the decline in the health-related quality of life for people with Parkinson’s.9
To best meet the needs of people living with Parkinson’s, both researchers and healthcare providers must learn to focus on the full experience of patients with Parkinson's disease, says Simona Sgarbi, PhD, researcher and senior real-world evidence lead at Lundbeck. Understanding exactly how patients' and care partners’ lives are affected by nonmotor symptoms, and how those symptoms impede their ability to live the lives they want will help the research community prioritize its goals. And it could help providers devise the most effective treatment regimens from the therapies that are available.
Putting patients at the center
To better understand the impact of nonmotor symptoms, Parkinson’s researchers at Lundbeck are gathering patient feedback at every stage of a research project. “We are mapping the patient experience across all stages of the disease, collecting both quantitative and qualitative information,” Sgarbi says. “We’re asking open-ended questions so that we get their real, lived experience and patients don’t have to fit their personal disease journey into catch-all categories.”
We recognize that while all patients aspire to a ‘normal’ life, each patient’s definition of ‘normal’ may differ. Understanding what people prioritize will help us design clinical trials with meaningful endpoints.”
— Simona Sgarbi, PhD, Lundbeck
Lundbeck also is partnering with patient advocacy organizations and other research institutions to map the Parkinson’s patient journey, forming patient-insight panels and seeking uniquely personal quality-of-life information. “We recognize that while all patients aspire to a ‘normal’ life, each patient’s definition of ‘normal’ may differ,” says Sgarbi. “It might be going to work, grocery shopping or meeting friends for coffee. Understanding what people prioritize will help us design clinical trials with meaningful endpoints.”
For example, Sgarbi explains, if a person is currently unable to meet friends out due to symptoms such as anxiety or incontinence, a meaningful endpoint for that patient might be meeting out at a café once a week. Another patient may not care about going out but would like to accomplish specific tasks connected with having friends over. According to Sgarbi, gathering this sort of highly personal patient feedback and conducting preference studies will help Lundbeck Parkinson’s researchers build a body of patient insights and incorporate the patient perspective into clinical trial design and drug development.
New era of Parkinson’s research
With the aging population, the number of Americans living with Parkinson’s is expected to swell to 1.2 million in 10 years.10 Considering the strong link between progression of nonmotor symptoms and quality of life, understanding how to better manage these symptoms will become vitally important.1
Historically, drug trials have been designed around improvement of a symptom, as measured on symptom-specific scales. While this method has produced effective and life-changing therapies for Parkinson’s, a truly patient-focused approach to Parkinson’s care will incorporate more of the patient perspective and consideration of patients’ quality of life. Working in collaboration with healthcare providers and listening intently to the needs of patients and care partners, Lundbeck is prepared to lead the next wave of patient-focused Parkinson’s research and drug development.
To learn more about managing neurogenic orthostatic hypotension (nOH), a non-motor symptom common in people with Parkinson’s disease and multiple system atrophy, visit nohmattershcp.com.
References
1. Poewe W, Seppi K, Tanner CM, et al. Parkinson’s disease. Nat Rev Dis Primers. 2017;3:17013.
2. Chaudhuri KR, Healy DG, Schapira AHV. Non-motor symptoms of Parkinson’s disease: diagnosis and management. Lancet Neurol. 2006; 5:235–45.
3. Barone P, Antonini A, Colosimo C, et al. The PRIAMO Study: a multicenter assessment of nonmotor symptoms and their impact on quality of life in Parkinson’s disease. Mov Disord. 2009;24(11):1641–1649.
4. Pont‐Sunyer C, Hotter A, Gaig C, et al. The onset of nonmotor symptoms in Parkinson's disease (The ONSET PDStudy). Mov Disord. 2014;30(2):229-237.
5. Aarsland D, Marsh L, Schrag A. Neuropsychiatric symptoms in Parkinson’s disease. Mov Disord. 2009;24(15):2175-2186.
6. Hurt CS, Rixon L, Chaudhuri KR, Moss-Morris R, Samuel M, Brown R. Barriers to reporting nonmotor symptoms to health-care providers in people with Parkinson’s. Parkinsonism Relat Disord. 2019;64:220-225.
7. Hatano T, Kubo SI, Shimo Y, Nishioka K, Hattori N. Unmet needs of patients with Parkinson's disease: interview survey of patients and caregivers. J Int Med Res. 2009;37(3):717-726.
8. Claassen DO, Adler CH, Hewitt LA, Gibbons C. Characterization of the symptoms of neurogenic orthostatic hypotension and their impact from a survey of patients and caregivers. BMC Neurol. 2018;18:125.
9. Martinez-Martin P, Rodriguez-Blazquez C, Kurtis MM, Chaudhuri KR. The impact of nonmotor symptoms on health-related quality of life of patients with Parkinson’s disease. Mov Disord. 2001;26(3):399-406.
10. Parkinson’s Foundation. Statistics. Available at https://www.parkinson.org/Understanding-Parkinsons/Statistics. Accessed 4/17/2020
©2020 Lundbeck. All rights reserved. UBR-C-100234.